surgery
Harry undergoes surgery
View more of Harry’s story below to see the outcome of his surgery.





to step down to the ward.

poor state,...


she would like “everything done”.

of ‘all active measures’.

and anticoagulation.

His daughter provides substitute consent for these interventions,
as his ‘person responsible’.





to step down to the ward.

poor state,...


she would like “everything done”.

of ‘all active measures’.

and anticoagulation.

His daughter provides substitute consent for these interventions,
as his ‘person responsible’.
Harry undergoes surgery to stabilise his fracture. Unfortunately, he has multiple post-operative complications including delirium, multiple pulmonary emboli and acute kidney injury. He spends a short time in intensive care post-operatively, then manages to step down to the ward. Despite maximal ward-based management, Harry remains in a clinically poor state, with ongoing delirium, multi-organ dysfunction, and fluctuating GCS.
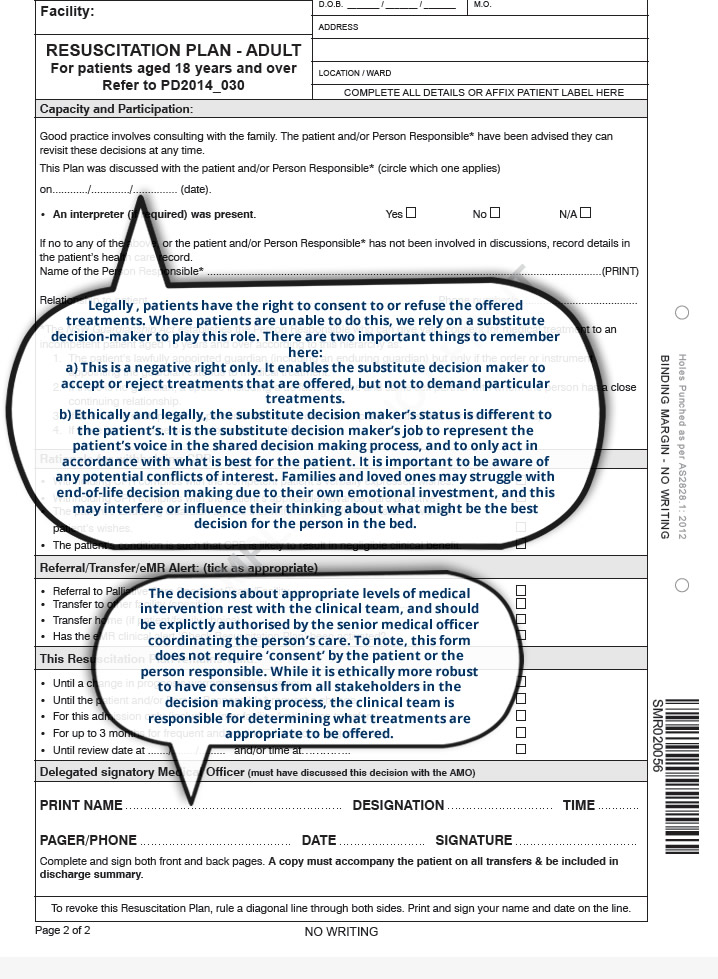
Harry’s daughter Margaret visits twice a week, and insists when asked that she would like “everything done”. The neurosurgical team document in the notes that he is for “all active measures”. This includes invasive tests, cannulas for IV fluid, albumin, antibiotics and anticoagulation. He is for full resuscitation measures, including escalation of care and CPR. His daughter provides substitute consent for these interventions, as his ‘person responsible’
Which other specialties do you think should be involved in Harry’s care at this juncture?
(Click on each option)
Consultation liaison psychiatry team
Consultation Liaison Psychiatry is commonly consulted when patients develop delirium, but this is not always necessary. They may have a particular role where there are challenging diagnostic issues, psychotic features, or where there is significant behavioural disturbance – Explore another option
Renal team
Seeking advice from subspecialty teams is important to identify what is going wrong, and how we may fix it. However, it is critical to remember that Harry’s outlook is determined by the whole picture as a sum of all parts, and not just by one specific organ or system pathology – Explore another option
Palliative care team
There is a potentially a role for palliative care involvement at this point. The goals of his surgery were always palliative, and he has a background of life limiting illness with multiple comorbidities. They may also be able to assist the team in focusing on Harry’s quality of life goals and symptoms – Explore another option
Respiratory team
Seeking advice from subspecialty teams is important to identify what is going wrong, and how we may fix it. However, it is critical to remember that Harry’s outlook is determined by the whole picture as a sum of all parts, and not just by one specific organ or system pathology – Explore another option
Harry’s prognosis
View more of Harry’s story below to see his progress.


advice relating to his respiratory and renal problems. Unfortunately, palliative care
were not consulted despite their input being indicated.

liaison psychiatry for advice and treatment regarding this.

treatments instituted.

of Harry recovering to independent living is very low.


who is in attendance on the ward at lunchtime.

invasive treatments, with a focus on symptom control and comfort.
The daughter becomes angry.





advice relating to his respiratory and renal problems. Unfortunately, palliative care
were not consulted despite their input being indicated.

liaison psychiatry for advice and treatment regarding this.

treatments instituted.

of Harry recovering to independent living is very low.


who is in attendance on the ward at lunchtime.

invasive treatments, with a focus on symptom control and comfort.
The daughter becomes angry.



One week on, Harry’s clinical status continues to worsen despite the treatments instituted. All consulting medical teams agree that his prognosis is poor, and the likelihood of Harry recovering to independent living is very low. At this stage he is still for all active measures, including CPR.
The team attempts to discuss Harry’s poor outlook with his daughter, who is in attendance on the ward at lunchtime. They broach the option of taking a more ‘conservative’ approach of less invasive treatments, with a focus on symptom control and comfort. Harry’s daughter becomes angry.
“How can you even say that? You are not giving up on him. Everything you have done has just made him worse. Now it’s your job to make him better! I want everything possible done to give him a chance.” She refuses to agree to a no CPR order when asked.
Now watch the following videos where Professor Ian Kerridge from Sydney Health Ethics discusses our obligations and the relevant ethical considerations in deciding what treatments should be offered in specific, sometimes complex, clinical situations.
Prof Ian Kerridge
“What obligations do we have in terms of what treatments should be offered to patients?
How do we understand these obligations where there is uncertainty or conflict about these decisions?”
Prof Ian Kerridge
“What are ‘futile’ treatments, and how can we understand this idea in the clinical setting?”